What are the advantages of embryo freezing?
As a policy, we transfer 1 embryo in women less than 35-yr old at the first or second IVF treatment cycle. For rare patients <35-yr old, failing to conceive with the first 2 IVF attempts, we may consider transferring two embryos. In women greater than 35-yr old, we transfer 1 or 2 embryos, following discussion with the couple. In pre-implantation genetic screening/testing (PGS/PGT) cycles, female age and the number of previous failed cycles lose their importance; hence, in such cases with highly filtrated embryos, we also transfer 1 embryo. Given the high maternal and neonatal risks associated with multiple pregnancies, we are very proud of our embryo transfer policy! Good and respectful clinics only transfer single embryo with high live birth rates!
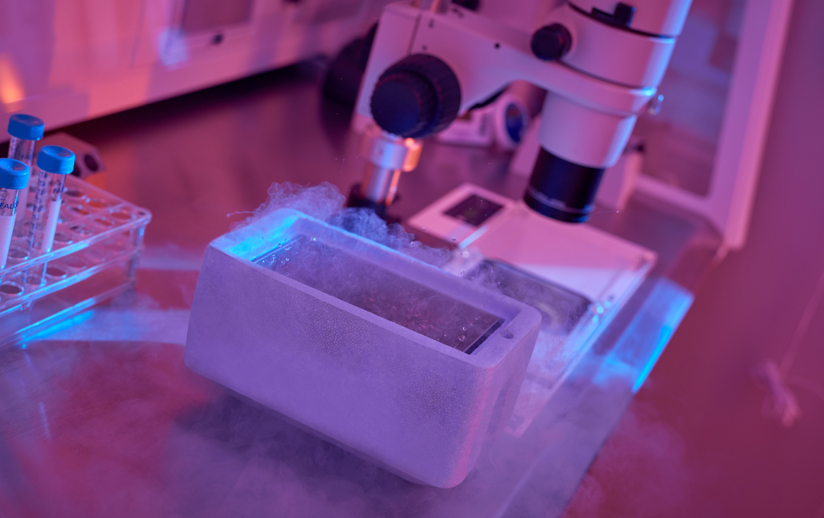
We have a very successful cryopreservation program for surplus embryos. We, currently, only freeze on Day 5 or 6 (5-6 days after OPU). Following thawing, the survival rate is around 98-100% and our pregnancy rates in frozen embryo replacement (FER) cycles is comparable to fresh Day 5 ET cycles, around 64%.
In the past, we used to freeze on Day 3; however, since the success rate is much higher with transfer of Day 5 embryos, we, nowadays, freeze only at the blastocyst stage (Day 5 or 6).
A FER cycle has several advantages, including i) the live birth rates are at least as good as those of fresh cycles (around 64%); ii) medications used to prepare the cycle is more friendly when compared to a fresh cycle; iii) no need for an oocyte-pick-up procedure; iv) since 1 embryo is transferred in the majority of cycles twin pregnancy is avoided given the high maternal and neonatal risks associated with multiple pregnancies.
How much is the chance of Success in procedure of Frozen Embryo Replacement (FER) Cycle?
We use vitrification method for freezing surplus embryos, which is currently the state-of-art method for freezing. Vitrification has been a breakthrough in IVF, given the very high (around 98-100% at our center) survival rates following thawing. The live birth rate in FER cycles is at least as good as those attained in fresh embryo transfer cycles. Even the live birth rates in FER cycles might be a little bit higher due to the lack of any detrimental effect of stimulation on the inner lining of the uterus in fresh cycles.
How the patient is prepared for the frozen embryo replacement cycle?
There are different protocols that may be employed for preparation of the inner lining of the uterus for a FER cycle. Those are;
- Completely natural cycle (with/without Crinone supplementation). This protocol is only performed in women with regular cycles. The only drawback of this protocol is the necessity of frequent trans-vaginal-ultrasonography and blood monitoring.
- Modified natural cycle (with/without Crinone supplementation). When the spontaneously developing follicle in a natural cycle attains a diameter of 16-20 mm, a single shot of medication (Ovitrelle) is given and embryo transfer is scheduled accordingly. This protocol is only performed in women with regular cycles. Compared to completely natural cycle, less monitoring is required.
- Artificial cycle with suppression. In this protocol, daily injections of Lucrin is commenced Day 21 of the preceding cycle; with menses oral estrogen pills (Cycloprogynova or Estrafem) and, thereafter, vaginal progesterone (Crinone) and intramuscular progesterone are started and embryo transfer is scheduled accordingly.
- Artifical cycle without suppression. With menses oral estrogen pills (Cycloprogynova or Estrafem) and, thereafter, vaginal progesterone (Crinone) and intramuscular progesterone are started and embryo transfer is scheduled accordingly.
We use all the given four protocols based on a personalized approach.
Apart from the availability of surplus embryos, we also freeze embryos in various circumstances, including;
- If we retrieve more than 15 oocytes, we wish not to make fresh embryo transfer and freeze all good-quality blastocysts. The reason for this is to avoid the so-called ovarian hyperstimulation syndrome (OHSS) risk. OHSS is a complication of ovarian stimulation, especially encountered in very good ovarian reserve patients (e.g. Polycystic ovary syndrome, polycystic ovary appearance). It is associated with fluid leakage from the vessels and hence fluid accumulation in potential spaces of the body (abdomen, thorax etc.). Systematic changes in other organ systems also accompany. Therefore, to avoid OHSS, we cancel the fresh cycle with such response. However, the quality of the eggs is not diminished with excessive response. Since we have a very reassuring vitrification program, with a cryo-all approach, we feel very confident in terms of success.
- In pre-implantation genetic screening/testing (PGS/PGT) cycles, we do not perform fresh embryo transfer and freeze all the biopsied blastocysts. The survival rate following vitrification is similar to non-PGS/PGT cycles and is around 98-100%.
- Rarely, with space occupying lesions in the uterine cavity, such as big polyps, we may go to freeze-all. In such cases, following hysteroscopic removal of such polyps, even at the time of oocyte pick-up, we may plan an immediate FER cycle, based on the availability of the patient.
- Finally, in fertility preservation cycles, we may go to freeze-all for the oocytes/embryos. Such cycles are performed in patients suffering from cancer (egg freezing). Starting from September 2014, egg freezing may be performed in unmarried females if they fulfill the conditions assigned by the Ministry of Health (cancer/diminished ovarian reserve or family history of early menopause).
Finally, we have a good freezing program for spermatozoa and testicular tissue when special circumstances defined by the Ministry of Health are met.